In a second experiment, she interrupts this steady resting breathing rate with a single, larger intake of air after approximately every fourth cycle of inspiration and expiration. When regular breathing resumes, the surface tension has fallen from 25 to 15. “We think that occasional deep breaths might be an important factor in reducing surface tension and making it easier to breathe,” Silva says.
To illustrate her point, Silva has prepared a presentation in the seminar room. She explains that our airways ramify more than 20 times, continuously dividing into smaller and smaller branches – from the trachea, bronchi and bronchioles all the way down to the alveoli. At the end of this respiratory tree, the alveoli form a network of several hundred million vesicles, connected by alveolar pores. These tiny air sacs inflate during inhalation and deflate during exhalation – and they are lined with surfactant to prevent them from collapsing after exhalation.
Deeper and Deeper
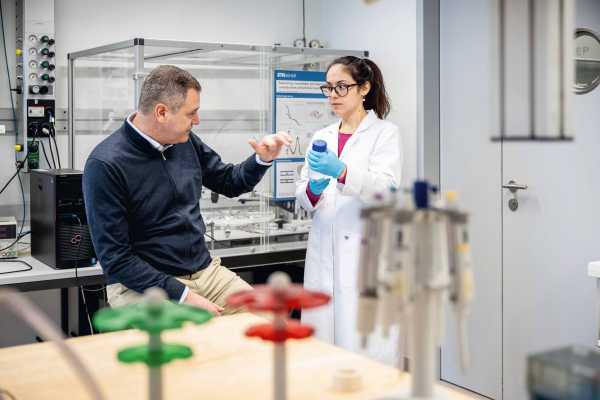
Back in the lab, Silva fills a different piece of equipment with animal surfactant. It resembles a giant spider with spindly silver legs. Suspended from its body hangs a thin needle, seemingly hovering over the surfactant. There is only a handful of these systems worldwide, all of which were developed in the ETH lab. Down in the basement, Silva’s goal was to simulate natural breathing: a few gentle breaths interspersed by the occasional deep one. Here, in the upstairs lab, the simulation is designed to mimic several softer resting breaths that gradually get deeper and deeper until they become a deep sigh. These expansions and contractions cause alterations in the surface area of the surfactant. The needle measures the surface tension throughout the experiment, allowing Silva to determine what happens as breathing becomes deeper. Currently, her results suggest that this expansion of the lungs is what reduces surface tension and makes breathing easier.
“Obviously, the situation in the lungs is much more complex!” she says, almost apologetically. “But as materials scientists, our task is to characterise the individual properties of a material as precisely as possible, so we deliberately attempt to untangle the complex interplay between the various forces.”
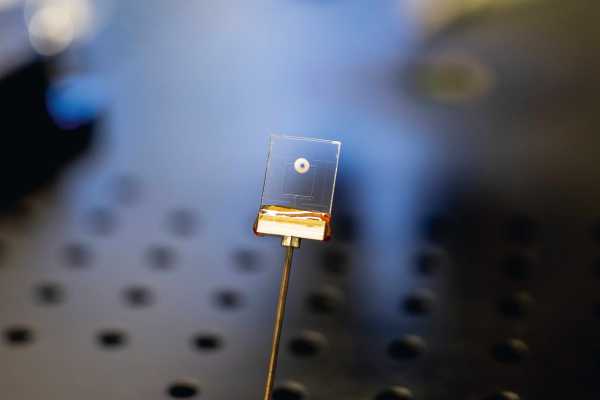
Silva still has one more piece of test equipment to put through its paces. Under the microscope is a small ring with a hole in the middle. It is surrounded by tiny pores and filled with surfactant. Using a special device, Silva applies pressure to the liquid. As she does so, the film gets thinner and eventually breaks. “Don’t worry, that’s meant to happen!” she says, smiling. During her presentation in the seminar room, she mentioned that alveoli are connected by pores. One possibility, she says, is that the thin film of surfactant breaks during breathing. This then equalises the pressure within the alveoli via the tiny pores between the vesicles.
Inject - or Inhale?
Silva is clearly fascinated by this mysterious fluid. But her experiments with surfactant are also motivated by the search for medical applications. These include the administration of surfactant to premature infants. Although this is often delivered as an injection, there are also non-invasive approaches that involve administering the surfactant as an aerosol via a breathing mask. “We hope our research will identify parameters that can improve this method,” says Silva. “By understanding the mechanisms at work here, we can help medical experts create even better tools.”
Silva knows what she’s aiming for – and she clearly has the perseverance, motivation and energy to achieve it.