New competence centre for personalised medicine in Zurich
DNA sequencing has revolutionised life sciences. Now it’s medicine’s turn: thanks to genetic analysis, treatment tailored to individual patients will be a standard feature in the future. With a new competence centre, ETH Zurich and the University of Zurich are aiming to lead the way in personalised medicine.
Niko Beerenwinkel, Professor of Computational Biology at ETH Zurich and Co-Director of the Competence Center for Personalized Medicine (CC-PM), which was established in April, is optimistic: “We are on the brink of a paradigmatic shift in medicine. The clinical application of personalised medicine is close to making a breakthrough.” Beerenwinkel believes that Zurich is the perfect place for this.
“In order to advance in personalised medicine we need clinical expertise, fundamental biological research and technological development. These lie just a stone’s throw away from each other here at University Hospital Zurich and ETH Zurich.” This is why, in 2013, researchers from the University of Zurich and ETH Zurich set up a joint competence centre.
This involved opening a new office at the University of Zurich for coordinating the combined efforts of the research groups involved, which themselves remain at their current sites. The office is being funded by the University of Zurich and ETH Zurich, each contributing CHF 0.5 million for the period from 2014 to 2017.
Bio-revolution driven by low-cost DNA decoding
Many experts believe that the future of medicine lies in personalisation. These days, institutes and research centres operating at the interface between medicine, biology and computer science can be found at almost any world-class university. This can be attributed to the tremendous progress made in DNA sequencing. In 2001 the scientific community celebrated as the human genome, which consists of 3.3 billion base pairs, was sequenced for the first time – the culmination of an eleven-year, three-billion-dollar project involving over two hundred scientists.
Nowadays, DNA sequencing is a standard procedure in biology, with the analysis of human DNA taking only a few days and costing less than CHF 5,000. This provides a powerful tool for medical professionals and biologists. For example, cancerous tumours are no longer identified by analysing tissue samples; instead, their genetic changes over time are described in detail. This is of vital importance, as although humans all have essentially the same DNA, the difference is in the detail. The smallest of variations in DNA control the differences in disease progression from person to person.
By measuring the genetic changes in a tumour, as well as the changes to cellular transcriptomes and proteomes, researchers are able to tailor treatment and increase the chances of recovery. Early versions of this personalised medicine have already been used successfully in lung cancer treatment.
The struggle to interpret mountains of data
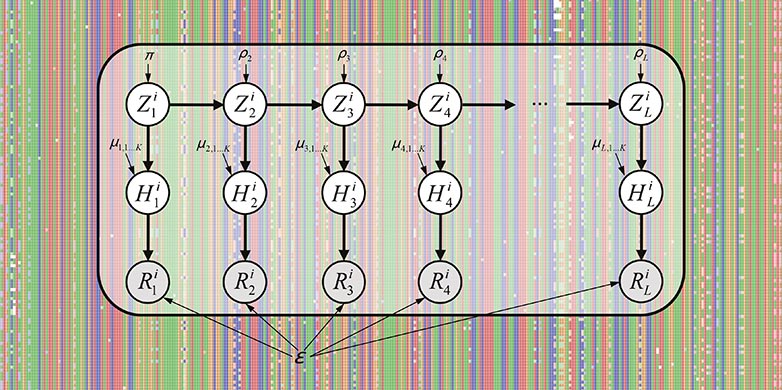
Now it is time for the next step: personalised medicine must find its way into daily clinical use. This presents new challenges for researchers and medical professionals: “The amount of data generated for genome sequencing is vast and very difficult to interpret,” explains Beerenwinkel. “In order to draw useful conclusions from this data, dedicated information systems are required, as well as new statistical and bioinformatic methods.”
To overcome these challenges, Holger Moch, Professor at the Institute of Surgical Pathology at the University of Zurich, and Wilhelm Krek, Professor of Cell Biology at ETH Zurich, established the CC-PM in 2013. In doing so, the existing expertise and resources of the two universities could be pooled and enhanced. “The research groups most heavily involved have already worked together in the past,” says Holger Moch, who, as the second Co-Director, is spearheading the CC-PM together with Niko Beerenwinkel. “Now we are building the institutional framework required for this kind of cooperation and paving the way for cross-institutional collaboration in the field of personalised medicine.”
In order to do this, three complementary technology platforms are being created within the CC-PM, with Holger Moch directing the Tissue, Sera and Cell Banking Technology Unit. This group is compiling an archive of well-characterised sample material, such as cell lines, tissue and sera (blood). Wilhelm Krek is leading the Theragnostics Discovery Unit, whose goal is an improved understanding of molecular disease mechanisms, while Niko Beerenwinkel’s Personalized Medicine ICT Unit is working on new concepts and software for managing and analysing the newly generated medical data.
Integration of DNA sequencing and patient data
Today, personalised medicine has made the most progress in oncology, i.e. the study of cancer. “In two years’ time, we will be able to sequence a large number of tumours even before cancer treatment has begun, and in five years this will be the norm,” predicts Beerenwinkel. Moch believes that, in the future, sufferers of diabetes and multiple sclerosis will also reap the benefits of improved treatment.
There are high hopes pinned on the integration of biologists’ genetic analyses with long-term data from clinical studies. By comparing patient data with thousands or even millions of entries in a database, researchers would be able to identify correlations between the genetic changes in tumours and patients’ symptoms. Based on the insights gained, treatment can be adapted to individual needs.
However, the security requirements for analyses like these are extremely high. “Complex anonymisation processes are needed in order to protect patients' privacy rights,” Beerenwinkel points out. The CC-PM also intends to focus its research on developing such processes.
New generation of medical professionals
The CC-PM should also benefit education, as it allows doctoral students to specialise in personalised medicine (Molecular and Translational Biomedicine) right from the start. Programmes for Bachelor’s and Master’s students are also planned for the future. Beerenwinkel is convinced that “we need a new generation of clinicians who know how to handle biomedical data.” Moch adds that “even now, medical professionals and bioinformaticians often don’t speak the same language. We need to promote mutual understanding in education.”
Photo gallery
-

Niko Beerenwinkel, Professor at ETH Zurich and Co-Director of the CC-PM. (Photo: ETH Zurich / Giulia Marthaler) -

Holger Moch, Professor at the University of Zurich and Co-Director of the CC-PM. (Photo: University of Zurich / Robert Huber) -

Wilhelm Krek, Professor at ETH Zurich and co-founder of the CC-PM. (Photo: ETH Zurich / Giulia Marthaler)